Vu Orthodontics - Orthodontics, Periodontics, and Implants
16027 Brookhurst St., Ste. K
Fountain Valley, CA 92708
ph: 714-775-0100
fax: 714-463-2205
drhungvu
- Home
- COVID-19 Notice
- CBCT
- CBCT & Chiropractic
- Biomechanics
- Services
- About Us
- Meet the Doctors
- Contact Us
- Cases
- Testimonials
- Emergency
- Office
- Ortho TADs
- Class II ("overbite")
- Class III ("underbite")
- Extremely Crowded
- Oral Surgery & Periodontics for GP
- Implants
- Medications
- Phlebotomy, PRF, PRP & SB
- Phase I (Pre-Teen Orthodontics)
- Adult Orthodontics
- Lasers
- Impacted Canines
- Accelerated Orthodontics
- Impacted Wisdom Teeth
- Referral Form
- Study Club
- Journal Articles
Ortho, Perio & Implants
Introduction
This section is a work-in-progress, devoted to periodontics and dental implants (hereinafter "implants"). The intended readers are general dentists (and other dentists) who are interested in periodontal surgery and implants.
Strong Topical Anesthetics
As an alternative to infiltration injection of local anesthetics, for some minimally invasive dental procedures, dentists can use strong topical anesthetics which are given as follows
- TAC 20% Alternate (20% lidocaine, 4% tetracaine, 2% phenylephrine)
- Profound (10% lidocaine, 10% prilocaine, 4% tetracaine)
- The Baddest Topical in Town (3% lidocaine, 12.5% prilocaine, 12.5% tetracaine, 3% phenylephrine)
- The Best Topical - EVER! (12.5% lidocaine, 12.5% tetracaine, 3% prilocaine, 3% phenylephrine)
where phenylephrine is a vaso-constrictor. Note that these strong topical anesthetics must not be allowed to stay on the soft tissue for long because they will cause the soft tissue to slough off.
Local Anesthetics
The two (2) most useful local anesthetics for use in dentistry are lidocaine and articaine.
1. Lidocaine (Xylocaine®) HCL 2% with epinephrine 1:100,000
Metabolism: Liver
Onset of action for infiltration anesthesia in dental patients: average, a bit less than 2 minnutes [1]
Elimination half-life: 1.5 h to 2 h
Duration of action (w/ epinephrine):
average, pulp anesthesia: ~1 hr [1]
average, soft tissue anesthesia: ~2 hr [1]
Excretion: Kidney
According to Collins et al [2], "lidocaine is known to have an onset <2 min, a duration of 1 h to 2 h, and a maximum dose of 5 mg/kg, which improves to an onset <2 min, a duration of 2 h to 6 h and toxicity of 7mg/kg with the addition of epinephrine. Each characteristic is dependent on multiple factors including volume and concentration infused, location of administration and tissue pH."
2. Articaine HCl 4% with 1:100 K epinephrine (Septocaine®)
Metabolism: Liver, plasma
Onset of action: within 1-9 minutes [3]
Elimination half-life: 0.5 hr
Duration of action: ~1 hr (infiltration) [3]
Excretion: Liver and unspecific plasmaestearases
According to Scully [4], "Articaine (carticaine) is an amide-type LA that has an onset and duration of anaesthesia similar to those of other intermediate acting amide LAs. The most significant benefit of articaine over lidocaine is that it may have somewhat faster onset and greater depth of action. Articaine is 1.5 times as potent and only 0.6 times as toxic as lidocaine and has beenshown to be superior in achieving successful anaesthesia following infiltration. It is not for injection in childrenunder 4 years of age. However, the use of inferior alveolar nerve blocks can be almost eliminated in children by using articaine due to its ability to anaesthetize teeth effectively by infiltration up to the first permanent molar region. In addition, diffusion of articaine on to the palatal surface may also eliminate the discomfort of palatal infiltration. It can also be used in patients taking beta-blockers. Articaine may be mildly neurotoxic and can cause prolonged anaesthesia, but its other adverse effects, toxic reactions and drug interactions (solutions containing a vasoconstrictor) are the same as those of other amide LAs (Table 3.9).The maximum recommended adult dose for articaine is 7 mg/kg. It should possibly not be given in porphyria."
According to Trott [5], "Articaine hydrochloride 4% (Septocaine) is an amide local anesthetic that has been used in Europe and other parts ofthe world for years and has now been approved for use in the United States. The only preparation available contains 1:100,000 epinephrine. Articaine is particularly effective in dental procedures because of its ability to penetrate hard tissues such as bone. It has yet to be studied for nondental procedures but can be used for facial and oral blocks. Onset of action is 1 to 6 minutes, and the duration of action is approximately 1 hour. Its safety profile is similar to other local 'caine' anesthetics."
According to Schug et al [6], "Nerve injury after mandibular nerve block has been previously reported. Articaine, and to a lesser extent prilocaine, has been implicated in an increased incidence of permanent paresthesia after mandibular nerve anesthesia, and lingual nerve injury is most common and most incapacitating. These conclusions have been supported by a recentcase series of 54 nerve injuries in 52 patients, in which standardized assessment of neurosensory function showed that toxicity was most likely the central causative factor... Over half of these cases were associated with the use of articaine. The authors concluded that articaine produced a more than 20-fold increase in the incidence of injection injury after mandibular nerve block. Recent reviewers have recommend avoiding articaine and prilocaine for mandibular and lingual nerve block, although they have concluded that it may be the high concentration rather the drug itself that is responsible for nerve damage."
3. Mepivacine HCl (Carbocaine™ )
Carbocaine™ 2% with Neo-Cobefrin 1:20,000 injection (mepivacaine HCl and levonordefrin injection, USP)
Mepivacaine (Carbocaine™) produces a mild vasoconstriction [7]; less vasodilation and has a more rapid onset and longer durationof action than lidocaine [9].
Type: Infiltration and Nerve Block, in adult sand pediatric patients [8]
Metabolism: extensively metabolized by the liver [9]
Onset of action: "the time of onset for sensory blockranging from about 3 to 20 minutes depending upon such factors as the anesthetic technique, the typeof block, the concentration of the solution, and the individual patient." [10]
"The onset of action is rapid (30 to 120 seconds in the upper jaw; 1 to 4 minutes in the lower jaw) [11]
Elimination half-life: "The half-life of CARBOCAINE (mepivacaine) in adults is 1.9 to 3.2 hours and in neonates 8.7 to 9 hours. Mepivacaine, because of its amide structure, is not detoxified by the circulating plasma esterases." [10]
Duration of action: "CARBOCAINE 3% injection will ordinarily provide operating anesthesia of 20 minutes in the upper jaw and 40 minutes in the lower jaw. CARBOCAINE 2% with Neo-Cobefrin 1:20,000 injection provides anesthesia of longer duration for more prolonged procedures, 1 hour to 2.5 hours in the upper jaw and 2.5 hours to 5.5 hours in the lower jaw." [11, bodlface added for emphasis]
Excretion: via the kidney [11]
Additional Notes:
(1) "CARBOCAINE (mepivacaine) containing a vasoconstrictor, such as epinephrine, should be used with extreme caution in patients receiving monoamine oxidase inhibitors (MAOI) orantidepressantsof thetriptyline or imipramine types, because severe prolonged hypertension may result." [10]
(2) "CARBOCAINE does not ordinarily produce irritation or tissue damage. Neo-Cobefrin is a sympathomimetic amine used as a vasoconstrictor in local anesthetic solutions. It has pharmacologic activity similar to that of Epinephrine but it is more stable than Epinephrine. In equal concentrations, Neo-Cobefrin is less potent than Epinephrine in raising blood pressure, and as a vasoconstrictor." [11]
4. Bupivacaine (Marcaine™, Sensorcaine™)
Type: Bupivacaine belongs to a class of drugs called Amides. It is not known if Marcaine™ is safe and effective in children younger than 12 years of age. (Source: https://www.rxlist.com)
Metabolism: primarily in the liver via conjugation with glucuronic acid.
Onset of Action: route and dose-dependent. The onset of action following dental injections can be from 1 to 17 minutes.
Elimination half-life: The half-life of Marcaine™ in adults is 2.7 hr and in neonates 8.1 hr. In clinical studies, elderly patients reached the maximal spread of analgesia and maximal motor blockade more rapidly than younger patients.
Duration of Action: long-acting. In dental use, bupivacaine (Marcaine™) may last 2 or 3 times longer than lidocaine (Xylocaine™) and mepivacaine (Carbocaine™), and in many patients up to 7 hr. The duration of anesthetic effect is prolonged by the addition of 1:200 K epinephrine.
Excretion: It has been reported to be excreted in human milk suggesting that the nursing infant could be theoretically exposed to a dose of the drug.
Other
Citanest (prilocaine) demonstrates no vasodilatory effect. [7]
Gingiva & Mucosa
In the mouth, keratinized tissue is gingiva and non-keratinized tissue is mucosa. Gingiva is tough, whereas mucosa is easy to tear. The border of mucosa and gingiva is called the mucogingival junction (MGJ). It may be easy to identify the MCJ on some patients, but that is not always the case.
Gingiva is divided into 2 types: free gingiva and attached gingiva. The coronal part of the gingiva from the cementoenamel junction (CEJ) is the free gingiva, where the apical part of the gingiva is the attached gingiva. For the most part, the free gingiva attaches to the enamel of the tooth by the junctional epithelium. The attached gingiva attaches to the root surface of the tooth by the connective tissue attachment.
Why are the distinctions important?
Many people suffer gingival recession, and one of most common causes is that these people tend to brush their teeth too hard. And the two most fundamental procedures for treating this condition is Free Gingival Graft (FGG) or Connective Tissue Graft (CTG). To be more precise, the latter is also called Subepithelium Connective Tissue Graft.
In FGG, the gingiva must be harvested as a superficial layer, the keratinized tissue, of the palate, whereas in CTG, the excised connective tissue is underneath the keratinized tissue of the palate.
In regeneration and soft tissue management, some common questions include the two controversial products: Emdogain (enamel matrix derivative, a product of Straumann) and AlloDerm Tissue Matrix (a skin product of LifeCell, distributed by BiHorizons).
References
1. Solutions for Local Anesthesia in Dentistry, Novocol Pharmaceutical of Canada, Inc. Cambridge, Ontario, Canada N1R 6X3
2. JB Collins, J Song, RC Mahabir. Onset and durationof intradermal mixtures of bupivacaine and lidocaine with epinephrine. Can J Plast Surg 2013;21(1):51-53.
3. Highlights of Prescribing Information. Septocaine® (articainehydrochloride and epinephrine injection), for intraoral submucosal infiltration use. Initial U.S. Approval: 2000. Novocol Pharmaceutical of Canada, Inc. Cambridge, Ontario, Canada N1R 6X3
4. C Scully CBE, MD, PhD, MDS, MRCS, FDSRCS, FDSRCPS, FFDRCSI, FDSRCSE, FRCPath, FMedSci, FHEA, FUCL, FBS, DSc, DChD, DMed (HC), Dr (hc). Perioperative Care, in Scully's Medical Problems in Dentistry (7th ed.), 2014
5. AT Trott. Infiltration and Nerve Block Anesthesia (Ch. 6), in Wounds and Lacerations (4th ed.), 2012
6. SA Schug, ... JHP Lau. Local anesthetics, in Side Effects of Drugs Annual, 2009
7. H H Lindorf, Investigation of the vascular effect of newer localanesthetics and vasoconstrictors, Oral Surg Oral Med Oral Pathol., 1979 Oct;48(4):292-7.doi: 10.1016/0030-4220(79)90026-4.
8. https://mms.mckesson.com/product/861424/CareStream-Health-1430735
9. https://www.pdr.net/drug-summary/Carbocaine-mepivacaine-hydrochloride-1238
10. https://www.rxlist.com/carbocaine-drug.htm#description
11. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=f00557a9-ec79-4c54-9d06-c71d2a8aff2c&type=display
Root Conditioning
The root of the tooth must be conditioned mechanically and chemically prior to certain grafting procedures. The process of cleaning the root mechanically will inevitably create a smear layer which must then be removed. The best way to remove this smear layer chemically is by using ethylenediaminetetraacetic acid (EDTA) which is an amino polycarboxylic acid, a chelating agent, and a colourless, water-soluble solid.
Traditionally, dentists and endodontists use EDTA solutions to remove the smear layer and lubricate the root canals in endodontics. The EDTA solution for this application is in a liquid form.
RC-Prep is routinely used for the chemo-mechanical preparation of root canals. Contents: 10 % urea-peroxide, urea peroxide and 15% EDTA in a paste form (special water-soluble base).
EDTA in a gel form is commercially available as PrefGel, a pH neutral, 24% EDTA, a product of Straumann. It is a root surface conditioner, for topical application onto exposed root surfaces.
Citric acid: Its use for root conditioning must be avoided because it is acidic and it may cause root resorption. Its pH is typically reported as 2.2, but this value varies depending on the concentration.
Sutures
Many types of sutures are used in surgical dentistry. Each type has pros and cons, and different dentists have different preferences. Sutures classified as monofilament or multifilament (braided) and absorbable or non-absorbable.
Some clinicians prefer smooth monofilament sutures for better healing (mainly by avoiding "wicking" effect of braided sutures).
The wicking of the multifilament sutures at the surgical sites often causes prolonged inflammatory reactions. Monofilament sutures are advantageous in preventing bacterial wicking into surgical sites.
The most common sutures are
- Plain gut: monofilament, absorbable, will last about 1 day in the oral environment
- Chromic gut: monofilament, absorbable, will last about 2 weeks in the oral environment
- Silk: multifilament, nonabsorbable, must be removed no more than about 10 days
More advanced sutures are
- PGCL (Poly Glycolide Co-Caprolactone): absorbable, synthetic. The thread is smooth and soft. Note that PGCL suture is similar to Monocryl® suture.
Thread type: Monofilament
Color: Violet/ Undyed
Strength duration: 14-21 days
Absorb duration: 90-120 days (Source: AD Surgical). But, in the experience of the author, some knots are generally broken in about 1 month.
- Polypropylene: monofilament, nonabsorbable, synthetic. It is indicated for soft tissue approximation and ligation. Its advantages include minimal tissue reactivity and durability. Disadvantages include fragility, high plasticity, and high expense. Prolene® is the most popular polypropylene suture. Note that nylon sutures are less expensive and are similar to polypropylene. But some clinicians report that Prolene is relatively more innert and less cutting soft tissue than nylon. But according to Wikipedia, "Prolene is a synthetic, monofilament, nonabsorbable polypropylene suture. It is indicated for skin closure and general soft tissue approximation and ligation. Its advantages include minimal tissue reactivity and durability. Disadvantages include fragility, high plasticity, high expense, and difficulty of use compared to standard nylon sutures."
- Polyglycolic acid (PGA): multifilament (braided) absorbable, synthetic, dyed and undyed. The thread is soft, and knot secured. Note that PGA suture is similar to Vicryl® suture.
- Polytetrafluoroethylene (PTFE) -- also known as Teflon®: nonabsorbable. Unlike most monofilament sutures, PTFE is soft. PTFE sutures may be considered as quasi-monofilament, so they prevent bacterial wicking, somewhat. But unlike PGCL or Prolene, PTFE sutures must not remain for long (at the surgical sites). Note that because of the streching characteristis, PTFE sutures lose their strength, so they are not as good as they were thought to be. There are three (3) different types of PTFE sutures:
1. e-PTFE (expanded PTFE): GORE-TEX suture which is porous but it is easier to handle (better knot stability)
2. d-PTFE (dense PTFE): Cytoplast suture is relatively stiff so it is more difficult to handle (better knot stability) but less porous than GORE-TEX
3. PTFE: Omnia PTFE suture -- According to the manufacturer, the suture is less porous than GORE-TEX and less stiff than Cytoplast.
Suture Needles
Two (2) important types of suture needles are discussed here: "conventional" cutting needle (Fig. 1) and "reverse" cutting needle (Fig. 2)
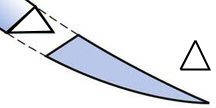
Fig. 1. Conventional Cutting Needle
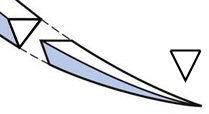
Fig. 2. Reverse Cutting Needle
“Conventional” cutting needles have the cutting edge on the concave surface (inner) and are useful for tough tissue, e.g., keratinized mucosa (masticatory mucosa which is keratinized stratified squamous epithelium).
On the other hand, “reverse” cutting needles have their cutting surfaces on the convex surface (outer) and are ideal for both tough tissue (e.g., keratinized mucosa) as well as delicate tissue (e.g., lining mucosa which is nonkeratinized stratified squamous epithelium).
Unlike conventional cutting needles, reverse cutting needles offer a reduced risk of cutting through tissue.
References
1. Michael S. Baggish, Suture Material, Suturing Techniques, and Knot Tying, Ch. 4
2. Oral Mucosa, Wikipedia
3. Szczepan Baran, Elizabeth Johnson, and Marcel Perret-Gentil, Understanding and Selecting Surgical Suture and Needle
4. Wayne W. LaMorte, Suturing Basics, Basics of Wound Closure and Healing
© Copyright 2007-2014, Vu Orthodontics. All rights reserved.
Serving communities: Orange County, Fountain Valley, Huntington Beach, Westminster, Garden Grove, Anaheim, Santa Ana, Buena Park, Tustin, Costa Mesa, Newport Beach, Irvine, Stanton, Cypress, Seal Beach, Los Alamitos, Fullerton, La Habra, Brea, Yorba Linda, Placentia, Villa Park, Lake Forest, Mission Viejo, Laguna Beach, Laguna Niguel, Laguna Hills; Los Angeles, Long Beach...
16027 Brookhurst St., Ste. K
Fountain Valley, CA 92708
ph: 714-775-0100
fax: 714-463-2205
drhungvu